The long struggle against diseases of all types includes acts of heroism by medical professionals, volunteers, and those stricken with illness. In the earliest days of inoculation against smallpox, using the smallpox virus itself in the hope of causing a weaker case of the illness and thus lifelong immunity, vaccination presented considerable risk. Those with compromised immune systems, a condition relatively unknown, risked death from vaccination. The number of deaths from vaccinations made many leery of the process for their children and loved ones. It took courage to trust the doctors who recommended inoculation.

Those seeking cures needed considerable courage as well. Close contact with victims suffering during wide outbreaks of yellow fever, malaria, influenza, and other diseases was deadly. Not until Louis Pasteur and others identified germs and microbes did washing hands and wearing protective clothing emerge. Some physicians and researchers deliberately placed themselves at even greater risk while seeking the sources of disease, and the means to cure them. Others relied on the courage of volunteers, who placed themselves at risk aware of the possibility of contracting a disease. Their reasons included patriotism, love of humanity, and in some cases monetary reward. Here are some heroes in the search for cures who placed their lives at risk for the benefit of others.
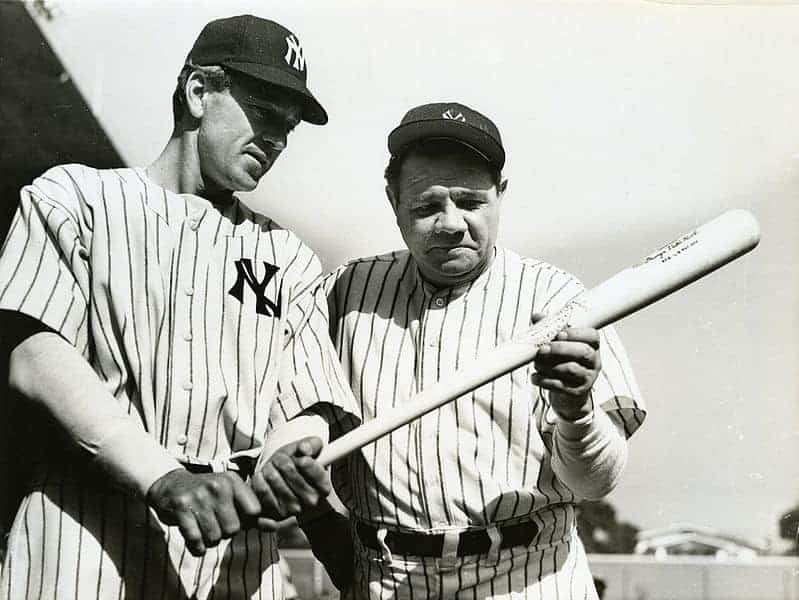
1. Dr. Jesse Lazear, US Army Yellow Fever Commission

Jesse Lazear trained at Johns Hopkins University and the Columbia University College of Physicians and Surgeons. He then completed his specialist training at the Pasteur Institute in Paris, before returning to Baltimore and Johns Hopkins. There he studied malaria and yellow fever from 1895 to 1900. That year he accepted an assignment as an assistant surgeon for the US Army at Quemados, Cuba. Assigned to the US Army Yellow Fever Commission, Lazear arrived in Cuba convinced of the work presented earlier by Carlos Finlay, that infected mosquitoes transmitted the disease to humans. In Cuba he set about to prove it, calling for volunteers to allow themselves to be infected.
According to Lazear’s own notes, discovered in 1947, the young surgeon and father of two deliberately allowed himself to be bitten by an infected mosquito. On September 8, 1900, Lazear wrote to his wife expressing confidence in his work. Just 17 days later he died of yellow fever. His act of deliberate infection was covered up in order that his family could collect on a life insurance policy. Lazear’s infection confirmed Finlay’s theory, but additional work regarding the spread of yellow fever continued under Walter Reed and others, to eliminate possible other sources of the disease. Johns Hopkins University named a dormitory to honor Lazear. He is also honored at the War Memorial Chapel at the National Cathedral in Washington DC.